The human colon may represent the most biodense ecosystem in the world. Though many may believe that our stool is primarily made up of undigested food, about 75 percent is pure bacteria—trillions and trillions, in fact, about half a trillion bacteria per teaspoon.
Do we get anything from these trillions of tenants taking up residence in our colon, or are they just squatting? They pay rent by boosting our immune system, making vitamins for us, improving our digestion, and balancing our hormones. We house and feed them, and they maintain and protect their house, our body. Prebiotics are what feed good bacteria. Probiotics are the good bacteria themselves. And postbiotics are what our bacteria make.
Our gut bacteria are known as a “forgotten organ,” as metabolically active as our liver and weighing as much as one of our kidneys. They may control as many as one in ten metabolites in our bloodstream. Each one of us has about 23,000 genes, but our gut bacteria, collectively, have about three million. About half of the cells in our body are not human. We are, in effect, a superorganism, a kind of “human-microbe hybrid.”
Having coevolved with us and our ancestors for millions of years, the relationship we have with our gut flora is so tightly knit as to affect most of our physiological functions. Yet our microbiome is probably the most adaptable component of our body. Gut bugs like Escherichia coli (E. coli) can divide every twenty minutes. The more than ten trillion bugs we churn out every day can therefore rapidly respond to changing life conditions. Every meal, we have the opportunity to nudge them in the right direction.
Thousands of years ago, Hippocrates is attributed as saying that all diseases begin in the gut or, more ominously, “death sits in the bowels.” Of course, he also thought women were hysterical because of their “wandering uterus.” (“Hysteria” comes from the Greek husterikos for “of the womb.”) So much for ancient medical wisdom. The pendulum then swung to the point of incredulity when the medical community refused to accept the role of one gut bug, Helicobacter pylori, as the cause of stomach and intestinal ulcers. Out of frustration, one of the pioneers chugged a brew of the bugs from one of his ulcer patients to prove the point, before finally being vindicated with the Nobel Prize in 2005 for his discovery.
In some ways, the pendulum has swung back, with overstated causal claims about the microbiome’s role in a wide range of disparate diseases that are casually bandied about. Perhaps the boldest such claim dates back more than a century to Élie Metchnikoff, who argued that senility and the disabilities of old age were caused by “putrefactive bacterial autotoxins” leaking from the colon. He was the first to emphasize the importance of the gut microbiome to aging. He attributed healthy aging to gut bacteria that fermented carbohydrates into beneficial metabolic end products like lactic acid and associated unhealthy aging with putrefaction, the process in which bacteria degrade protein into noxious metabolites as waste products.
There is no shortage throughout history of oldtimey crackpots with quack medical theories, but Metchnikoff was no slouch. He was appointed Louis Pasteur’s successor, coined the terms “gerontology” and “probiotics,” and won the Nobel Prize in medicine to become the founding “father of cellular immunology.” More than a century later, some aspects of his theories on aging and the gut are now being vindicated.
Young at Gut
Full-term, vaginally delivered, breastfed babies are said to start out with the gold standard for a healthy microbiome, which then starts to diverge as we age. The microbiomes of children, adults, the elderly, and centenarians tend to cluster together, such that a “microbiomic clock” can be devised. Dozens of different classes of bacteria in our gut so reliably shift as we age that our age can be guessed based on a stool sample within about a six-year margin of error. If these changes turn out to play a causal role in the aging process, then, hypothetically, our future high-tech toilet may one day be able predict our lifespan as well.
The transition from adulthood into old age is accompanied by pronounced changes to the microbiome. Given large interpersonal differences, there is no “typical” microbiome of the elderly, but the trends are in the very direction Metchnikoff described: a shift from the fermentation of fiber to the putrefaction of protein. This deviation from good bugs to bad is accompanied by an increase in gut leakiness, the spillage of bacterial toxins into the bloodstream, and a cascade of inflammatory effects. This has led to the proposal that this microbiome shift is a “primary cause of aging-associated pathologies and consequent premature death of elderly people.”
The most important role a healthy microbiome has for preserving health as we age is thought to be the prevention of systemic inflammation.
As profound a change in microbiome composition from early adulthood into old age, there’s an even bigger divergence between the elderly and centenarians. When researchers analyzed centenarian poop, they found a maintenance of short-chain fatty acid production from fiber fermentation. For example, in the Bama County longevity region in the Guangxi province of China, fecal sample analyses found that centenarians were churning out more than twice as much butyrate as those in their eighties or nineties living in the same region. Butyrate is an anti-inflammatory short-chain fatty acid critical for the maintenance of gut barrier integrity. At the same time, there were significantly fewer products of putrefaction, such as ammonia and uremic toxins like p-cresol. The researchers concluded that an increase of dietary fiber intake may therefore be a path toward longevity. An abundance of fiber feeders also distinguished healthy individuals ninety years and older from unhealthy nonagenarians.
Centenarian Scat
Interestingly, the microbiomes of Chinese centenarians shared some common features with Italian centenarians, suggesting that there could be certain universal signatures of a longevity-promoting microbiome. For example, centenarians have up to about a fifteenfold increase in butyrate producers.
A study of dozens of semi-supercentenarians (those aged 105 to 109) found higher levels of health-associated bacteria, such as Bifidobacteria and Akkermansia. In vaginally delivered, breastfed infants,
Bifidobacteria make up 90 percent of colon bacteria, but the level may slip down to less than five percent in adult colons and even less in the elderly and those with inflammatory bowel disease. But centenarians carry more of the good bacteria in their gut.
Bifidobacteria are often used as probiotics, but anti-aging properties may exist in their postbiotics. Bifidobacteria are one of the many bacteria that secrete “exopolysaccharides,” a science-y word for slime. That’s what dental plaque is—the biofilm created by bacteria on our teeth. Exopolysaccharides produced from a strain of Bifidobacteria isolated from centenarian poop were found to have anti-aging properties in mice, reducing the accumulation of age pigment in their brains and boosting the antioxidant capacity of their blood and livers.
Akkermansia muciniphila is named after the late Dutch microbiologist Antoon Akkermans and from Latin and Greek for “mucus-lover.” The species is the dominant colonizer of the protective mucus layer in our gut that is secreted by our intestinal lining. Unfortunately, that mucus layer thins as we age, a problem exacerbated by low-fiber diets. When we eat a fiber-depleted diet, we starve our microbial selves. Our famished flora, the microbes in our gut, have to then compete for limited resources and may consume our own mucus barrier as an alternative energy source, thereby undermining our defenses. Mucus erosion from bacterial overgrazing can be switched on and off on a day-to-day basis in mice supplanted with human microbiomes with fiber-rich and fiber-free diets. You can even show it in a Petri dish. Researchers successfully recreated layers of human intestinal cells and showed that dripping fiber (from plantains and broccoli) onto the cells at dietary doses could “markedly reduce” the number of E. coli bacteria breaching the barrier. Aside from eating fiber-rich foods, A. muciniphila helps to directly restore the protective layer by stimulating mucus secretion.
A. muciniphila is a likely candidate for a healthy aging biomarker, as its abundance is enriched in centenarians and it is particularly scarce in elders suffering from frailty. A comparative study was undertaken of the microbiomes of people in their seventies and eighties experiencing “healthy” versus “non-healthy” aging, defined as the absence or presence of cancer, diabetes, or heart, lung, or brain disease. Akkermansia, the species most associated with healthier aging, were three times more abundant in the fecal samples of the healthy versus non-healthy aging cohort. Among centenarians, a drop in A. muciniphila is one of the microbiome changes that seems to occur about seven months before death, despite no apparent changes in the physical status, food intake, or appetite at the time. To prove a causal role in aging, researchers showed that feeding A. muciniphila to aging-accelerated mice significantly extended their lifespans.
Cause, Consequence, or Confounding
A recurring recommendation from centenarian poop studies is the promotion of high-fiber diets, one of the most consistently cited pieces of lifestyle advice in general for extreme longevity and health. An alternative proposal is a fecal transplant, from a cocktail of centenarian stool. Both approaches assume a cause-and-effect relationship between fiber-fueled feces and long lives, but there remains much controversy over whether age-related microbiome changes are cause, consequence, or confounding.
Aging is accompanied by dysbiosis, an unhealthy imbalance of gut flora characterized by a loss of fiber-fed species. Rather than a changing microbiome contributing to the aging process, it’s easier to imagine how aging could instead be contributing to a changing microbiome. Loss of taste, smell, and teeth with age could lead to decreased consumption of fiber-rich foods, replaced by salted, sweetened, easier-to-chew processed foods. The drop in the quantity and diversity of whole plant foods—the only naturally abundant source of fiber—could result in a dysbiosis that leads to early death and disability. Or, the decline in diet quality could directly dispose to disease, with the dysbiosis just an incidental marker of an unhealthy diet.
There are also ways aging can be connected to dysbiosis independent of diet. While the rates of antibiotic prescriptions in childhood and through middle age have dropped in recent years, prescription rates among the elderly have shot up. Even non-antibiotic pharmaceuticals can muck with our microbiome. A study pitting more than a thousand FDA-approved drugs against forty representative strains of gut bacteria found that 24 percent of marketed drugs inhibited the growth of at least one strain. Reduced physical activity could also contribute to sluggish, stagnant bowels that could leave our gut bugs no other choice but to turn to protein for putrefaction once preferred prebiotics are used up. Nursing home residents are often fed the kind of low-fiber diet that can contribute to the “decimation” of a healthy microbiome.
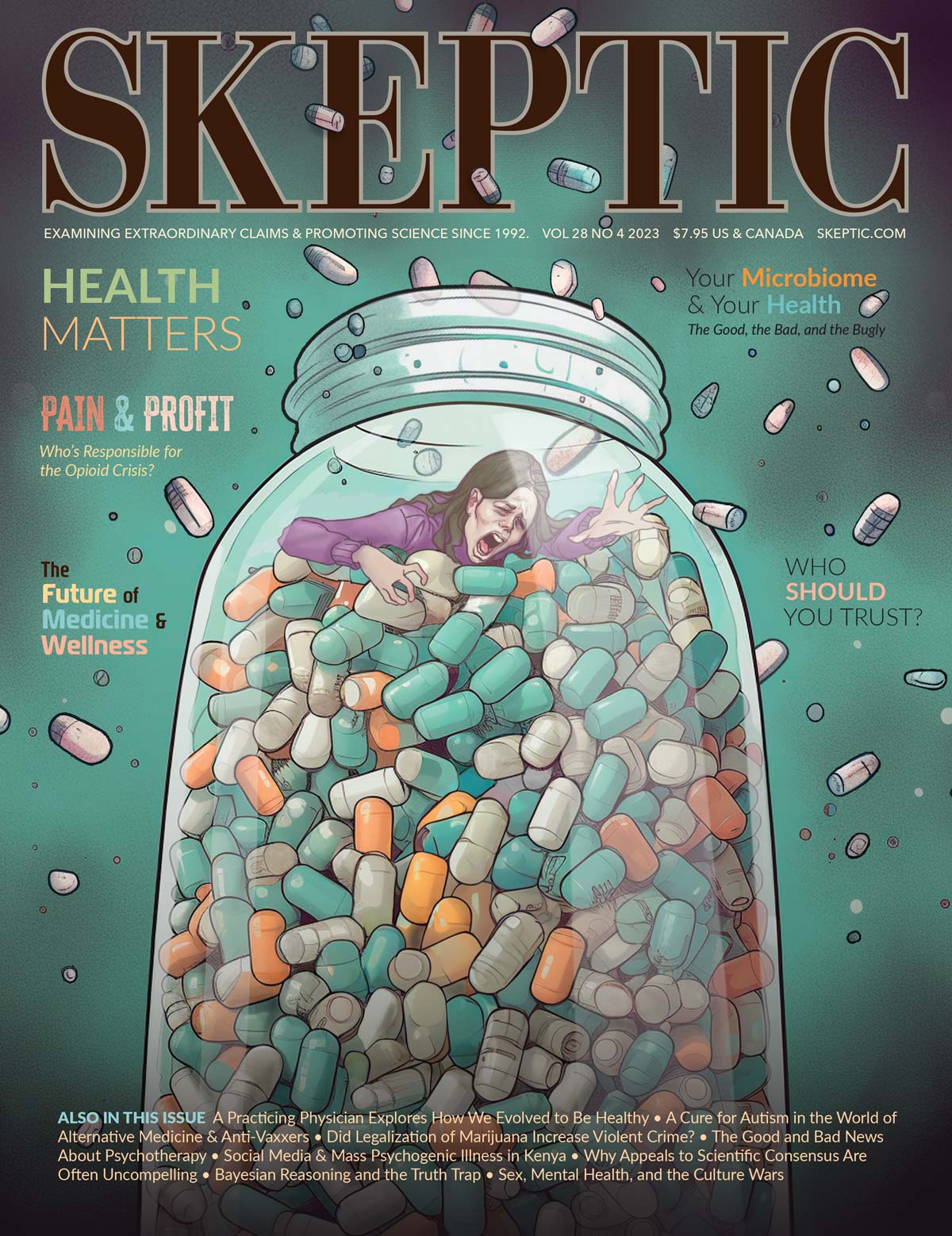
This article appeared in Skeptic magazine 28.4
Buy print edition
Buy digital edition
Subscribe to print edition
Subscribe to digital edition
Download our app
So, while researchers have interpreted the link between dysbiosis and frailty as a poor diet leading to poor gut flora leading to poor health, the arrows of causality could potentially go in every which direction. Maybe there’s even a chicken-or-the-egg feedback loop in play. With so many interrelated factors, you can imagine how hard it is to tease out the causal chain of events.
These questions crop up all the time in microbiome research. For example, the microbiomes of centenarians aren’t just better at digesting fiber. They’re better at detoxifying industrial pollutants, such as petrochemicals; food preservatives like benzoate and naphthalene, used in petroleum refinement; and haloalkanes, widely used commercially as flame retardants, refrigerants, propellants, and solvents. None of these detoxification pathways was found in the microbiomes of the Hadza, one of the last hunter-gatherer tribes in Africa. Did the enhanced detoxification in centenarian guts (compared to younger individuals) contribute to their longevity, or did their longevity contribute to their enhanced detoxification (given their longer lifetime exposure and accumulation of chemicals)?
The microbiomes of centenarians and semi-supercentenarians are better able to metabolize plant fats than animal fats, but maybe that’s just due to their eating more plant-based diets. The Bama County longevity region centenarians who had such an abundance of fiber feeders were eating more than 70 percent more fiber (38 g versus only 22 g per 2,000 calories) compared to those aged eighty through ninety-nine living in the same region. The only way to know if their longer lives eating more healthfully just led to a better microbiome or if their better microbiome actually contributed to their living longer is to put it to the test.
Fecal Transplant Experiments
Longevity researchers have good reason to suspect a causal, rather than bystander, role for age-related microbiome changes, given fecal transplant studies showing that the lives of old animals can be extended by receiving gut bugs from younger animals. Centenarian stool has anti-aging effects when fed to mice. Researchers fed mice fecal matter from a 70-year-old individual that contained Bilophila wadsworthia, a pro-inflammatory bacteria enriched by a diet high in animal products, versus feces from a 101-year-old containing more fiber feeders. Mice transplanted with the centenarian microbiome ended up displaying a range of youthful physiological indicators, including less age pigment in their brains. This raises the possibility that we will one day be using centenarian fecal matter to promote healthy aging. Why bathe in the blood of virgins when you can dine on the dung of the venerable?
Plugging Leaks with Fiber
One of the mechanisms by which intestinal dysbiosis may accelerate aging is a leaky gut. This can lead to tiny bits of undigested food, microbes, and toxins slipping through our gut lining and entering uninvited into our bloodstream, triggering chronic systemic inflammation. Thankfully, there’s something we can do about it.
To avoid gut dysbiosis, inflammation, and leakiness, plants should be preferred. The reason vegetarians tend to have a better intestinal microbiome balance, a high bacterial biodiversity, and enhanced integrity of the intestinal barrier, and also produce markedly less uremic toxins in the gut, is likely that fiber is the primary food for a healthy gut microbiome. Cause and effect was established in a randomized, double-blind, crossover study of pasta with or without added fiber.
Dysbiosis Inflammation Immunosuppression
The most important role a healthy microbiome has for preserving health as we age is thought to be the prevention of systemic inflammation. Inflammaging is a strong risk factor not only for premature death. Those with higher-than-average levels of inflammatory markers in their blood for their age are more likely to be hospitalized, frail, and less independent, and suffer from a variety of diseases, including common infections.
In Japan, for example, more than 40 percent of all centenarian deaths are due to pneumonia and other infectious diseases. In one of the largest studies, involving nearly 36,000 British centenarians, pneumonia was the leading identifiable cause of death. Inflammaging has not only been shown to increase susceptibility to coming down with the leading cause of bacterial pneumonia but older adults with more inflammation also tend to suffer increased severity and decreased survival.
As we age, our immune system macrophages (from the Greek for “big eaters”) start to lose their ability to engulf and destroy bacteria. The same happens in regular mice. But mice raised microbe-free don’t suffer from the leaking gut, subsequent inflammation, and loss of macrophage function. To connect the dots between the inflammation and loss of function, researchers found that the macrophage impairment could be induced in microbe-free mice by infusing them with an inflammatory mediator, which, when dripped on macrophages in a Petri dish, could directly interfere with their ability to kill pneumonia bacteria. Because our immune system is also responsible for cancer defense, immune dysfunction caused by the inflammation resulting from dysbiosis may also help explain why cancer incidence increases so steeply as we age (and why microbe-free mice have fewer tumors and live longer).
Avoiding Dietary Antibiotics
Other than getting enough fiber, what else can we do to prevent dysbiosis in the first place? There are a number of factors that contribute to microbiome imbalance. For example, on any given day, an average of about two and a half doses of antibiotics are consumed for every one hundred people in Western countries. The havoc this can play on our microbiome may explain why antibiotic use predicts an increased risk of cancer, though confounding factors, such as smoking, that are associated with both, could also potentially explain this link.
Up to three-quarters of antibiotic use is of questionable therapeutic value. Avoiding unnecessary use of antibiotics and using targeted, narrow-spectrum agents whenever possible can help protect our gut flora, but most people may not realize they’re consuming antibiotic residues every day in the meat, dairy, and eggs they eat. As much as 80 percent of the antibiotics used in the United States doesn’t go to treat sick people but rather is fed to farm animals in part as a crutch to compensate for the squalid conditions that now characterize much of modern agribusiness. But do enough antibiotics make it onto our plates to make a difference?
Infections with multidrug-resistant bacteria are on target to become the world’s leading cause of disease and death by the year 2050, poised to surpass even cancer and heart disease. Excessive antibiotic use can result in our guts becoming colonized with these superbugs, so researchers set out to calculate how many animal products one would need to eat to achieve antibiotic concentrations in our colon to give resistant bugs an advantage. Single servings of beef, chicken, or pork were found to contain enough tetracycline, ciprofloxacin, tilmicosin, tylosin, sarafloxacin, and erythromycin to favor the growth of resistant bacteria. One and a half servings of fish (150 g) exceeded minimum selective concentrations of ciprofloxacin and erythromycin. Two cups of milk could tip the scales for tetracycline, ciprofloxacin, tilmicosin, tylosin, and lincomycin. And, legal levels of erythromycin and oxytetracycline in two eggs could also exceed safe levels.
We need to stop squandering lifesaving miracle drugs just to speed the growth of farm animals reared in unhygienic conditions, and we also need to stop the reckless overuse in medicine. ![]()
Excerpted from How Not to Age: The Scientific Approach to Getting Healthier as You Get Older by Michael Greger. Copyright © 2023 by Michael Greger. Reprinted with permission from Flatiron Books. All rights reserved.
About the Author
Michael Greger, M.D. FACLM is a graduate of the Cornell University School of Agriculture and the Tufts University School of Medicine. He is a practicing physician and author of Bird Flu: A Virus of Our Own Hatching and Carbophobia: The Scary Truth Behind America’s Low Carb Craze. Three of his recent books—How Not to Die, the How Not to Die Cookbook, and How Not to Diet—became instant New York Times Best Sellers. Greger has lectured at the Conference on World Affairs and the National Institute of Health, testified before Congress, and appeared on shows such as The Colbert Report and Oprah Winfrey.
This article was published on February 1, 2024.