White Coat Crime
She murdered her patients. At least, that’s what the prosecutors said. All it took to get powerful opioids from California internist Lisa Tseng was a brief conversation. No X-rays. No lab tests. No medical exam. Video surveillance shows an undercover officer posing as a patient who asks Dr. Tseng for methadone (an opioid) and Xanax (an anti-anxiety medication), drugs that can form a deadly cocktail when combined. He tells her that he is in recovery and takes the drugs at night with alcohol to “take the edge off.” He makes clear that he is not in pain and does not plan to use the medications to treat a medical condition. Tseng writes the prescription—after the agent hands over $75 cash.1
Did she know what she was doing was wrong? Tseng received desperate calls from patients’ families and friends concerned that their loved ones were hooked on the meds she prescribed.2 She did not stop. Coroners and law enforcement agents called Dr. Tseng each time a patient died—14 in total.3 She did not stop. Perhaps she thought the financial perks outweighed the risks. Dr. Tseng’s reckless prescribing raked in $3,000 a day and exceeded $5 million in three years.
Dr. Tseng’s prescribing spree ended in 2015, when a jury convicted her on three counts of second-degree murder.4 In 2016, Superior Court Judge George G. Lomeli imposed a prison sentence of 30 years to life in prison. The trial lasted eight weeks. It included 77 witnesses and 250 pieces of evidence. Families of overdose victims praised the judge’s decision and concluded that “justice has been served.”5
Dr. Tseng was the first California physician ever convicted of murder for overprescribing opioids, and one of the first in the United States. Her case was a turning point for law enforcement because it created a playbook for subsequent prosecutions and because it sent a clear signal to physicians across the nation: you could be next. “The message this case sends is you can’t hide behind a white lab coat and commit crimes,” declared Deputy District Attorney John Niedermann. “A lab coat and stethoscope are no shield.” Medical experts warned that Tseng’s case could scare physicians away from prescribing opioids and leave chronic pain patients to suffer without care.6

Law enforcement is responsible for making sure that doctors only prescribe opioids legally, which is no easy task. However, some physicians make it easy when they engage in behavior that is explicitly and undeniably criminal. These are the cases that make headlines. Opioids are illegal by default. Federal law gives doctors a special exemption to prescribe them for legitimate medical purposes, particularly pain. But how can a physician be legitimate if he has a parking lot filled with out-of-state license plates and a line of patients snaking around the building as if they are waiting to buy concert tickets? If he asks the patient to state his blood pressure while a brand-new blood pressure cuff hangs on the wall, unused? If he can’t tell the difference between a dog X-ray and a human one?
Doctors are hard to investigate and even harder to prosecute. It is difficult for judges and juries to wrap their minds around the idea that physicians perpetrate crimes.
It sounds far-fetched, but in July 2012, Glendora, CA, police arrested physician Rolando Lodevico Atiga for prescribing powerful opioids to an undercover officer. The officer used a dog X-ray—with the tail clearly visible—to prove he had a bad back. Police Captain Tim Staab told CBS, “Either Sparky the dog really needs Percocet or this doctor is a drug dealer masquerading as a physician.”7 The medical board suspended Dr. Atiga’s license in August 2012.8 Then criminal proceedings were suspended in 2013 due to Dr. Atiga’s poor mental health and inability to stand trial.9
Doctors are hard to investigate and even harder to prosecute. It is difficult for judges and juries to wrap their minds around the idea that physicians perpetrate crimes. The image of the “dirty doctor” just doesn’t mesh with the popular image of “doctor as savior.” And many overdoses involve multiple drugs, making it hard to pin a death on a single drug or a single doctor.10 Still, over the past decade, judges and juries have put physicians behind bars. Law enforcement arrests scores of physicians for opioid crimes each year. They charge physicians with the same counts as illicit drug dealers: fraud, unlawful distribution, racketeering, manslaughter, and murder.11 Doctors are legally required to keep extensive records that investigators use to prove criminal activity. Physicians who avoid arrest still face steep penalties, such as losing their medical license, losing the ability to prescribe controlled substances, or paying a hefty fine.

It was not always this way. As early as the mid-1990s, evidence showed that physicians were generously doling out opioids, but the first murder conviction did not occur until 2016.12 What happened over those twenty years that unleashed prosecutors’ power and helped them win cases against providers? The answer lies in organizational change, education, and technological innovation. New organizations centered on criminal healthcare providers cropped up, enforcement agents came together to share strategies, and Prescription Drug Monitoring Programs (PDMPs) spread across the nation that made targeting physicians a far easier task.
Reshaping the Enforcement Landscape
A lot has changed since the days when pill mills popped up like weeds and law enforcement had no way to stop them. Enforcement agencies have responded to the opioid crisis with three strategies: (1) organizing task forces, (2) educating investigators, and (3) using PDMPs. Together, these efforts have made physician cases easier and faster to initiate, even if some challenges persist.
Task forces are subunits of enforcement agencies that bring together individuals who have different resources and expertise to address a common goal. Federal agencies such as the Drug Enforcement Administration (DEA) and local agencies such as sheriffs’ departments have devoted themselves to physician cases by creating task forces centered on prescription opioids. DEA task forces do much of the heavy lifting, a major difference from decades ago.
The DEA plays the biggest federal role in regulating opioids. The DEA’s Office of Diversion Control oversees registrants—physicians, pharmacies, hospitals, manufacturers, wholesalers, and drug distributors—who must register with the agency in order to provide controlled substances. The Controlled Substances Act (CSA) designates these registrants as part of a “closed system of distribution,” which means that the DEA tracks everyone who handles opioids along the supply chain and accounts for every transaction. The DEA monitors opioid transactions using the Automation of Reports and Consolidated Orders System (ARCOS), a database that tracks controlled substances all the way from manufacture to public distribution.13
“The message this case sends is … a lab coat and stethoscope are no shield.”
—Deputy District Attorney John Niedermann
For decades, the Office of Diversion Control14 was considered a lesser part of the DEA, and the agents who worked for it—known as Diversion Investigators (DIs)—were treated as less important than Special Agents (SAs), who work for the Operations Division. The position of DI was originally created to relieve SAs from the burden of inspecting and auditing manufacturers and distributors of controlled substances as mandated by the CSA. Handing off those tasks to DIs freed SAs to focus on heroin and cocaine trafficking. This hierarchy persisted into the late 1990s, the heyday of opioid prescribing, when physicians treated pain as a fifth vital sign and were urged to treat it aggressively. With physicians and regulators on board with generous opioid prescribing, the diversion office found itself underfunded and understaffed. Laura Nagel, who was appointed head of the DEA’s Office of Diversion Control in 2000, led DIs who struggled to get resources and respect. Unaware of the giant opioid wave poised to crest a few short years later, SAs thought prescription opioids were nothing more than a child’s version of the hard drugs they pursued.
That all changed in the early 2000s when, for the first time in U.S. history, Americans were more likely to overdose on prescription drugs than illegal ones.15 Suddenly, DIs were in high demand. In late 2006, the DEA created task forces called Tactical Diversion Squads. These included DIs, SAs, and Task Force Officers (TFOs), who are local police deputized to work with the DEA. DIs understood healthcare norms; SAs could arrest people; and TFOs had fine-grained knowledge of their communities. This arrangement created the organizational synergy needed to pursue doctors.
Local agencies such as police departments and sheriff’s departments also created narcotics task forces that enabled them to exchange information with other local agencies. Members of such task forces can represent various police departments, the highway patrol, the district attorney’s office, the department of healthcare services, and the medical board. They may also ally with the FBI, the DEA, and the Food and Drug Administration (FDA).
Federal and local agencies have complementary resources. Local police departments have insufficient funding to do provider cases, so they collaborate with federal law enforcement either formally by sending one of their officers to the DEA’s task force or informally by working cases with them. Federal agencies have more money and equipment. They can perform federal wire taps, which are expensive and require specialized technology. They can also afford expert witnesses, whose expertise is crucial in building a solid case against a doctor. Local agencies, on the other hand, have more agents, so they are better equipped to conduct undercover investigations and process the mountains of paperwork that a doctor case generates.
Prescription Drug Monitoring Programs (PDMPs) have dramatically transformed the ways that investigators and prosecutors conduct cases against providers.
Task forces are only one site of information exchange. Enforcement agents have found various ways to break down information silos and thereby distribute knowledge. Years of failed attempts have taught investigators and prosecutors both what works, and what doesn’t. They know which questions to ask, which behaviors to look for, and which charges to bring. When task force members, eager to share what they had learned with others, lacked formal venues in which to do so, they got creative.
Together, new organizations, new knowledge, and new technology expand law enforcement capacity. These changes are evident when we consider what investigation and prosecution look like today. Let’s turn to PDMPs as an example.
Prescription Drug Monitoring Programs
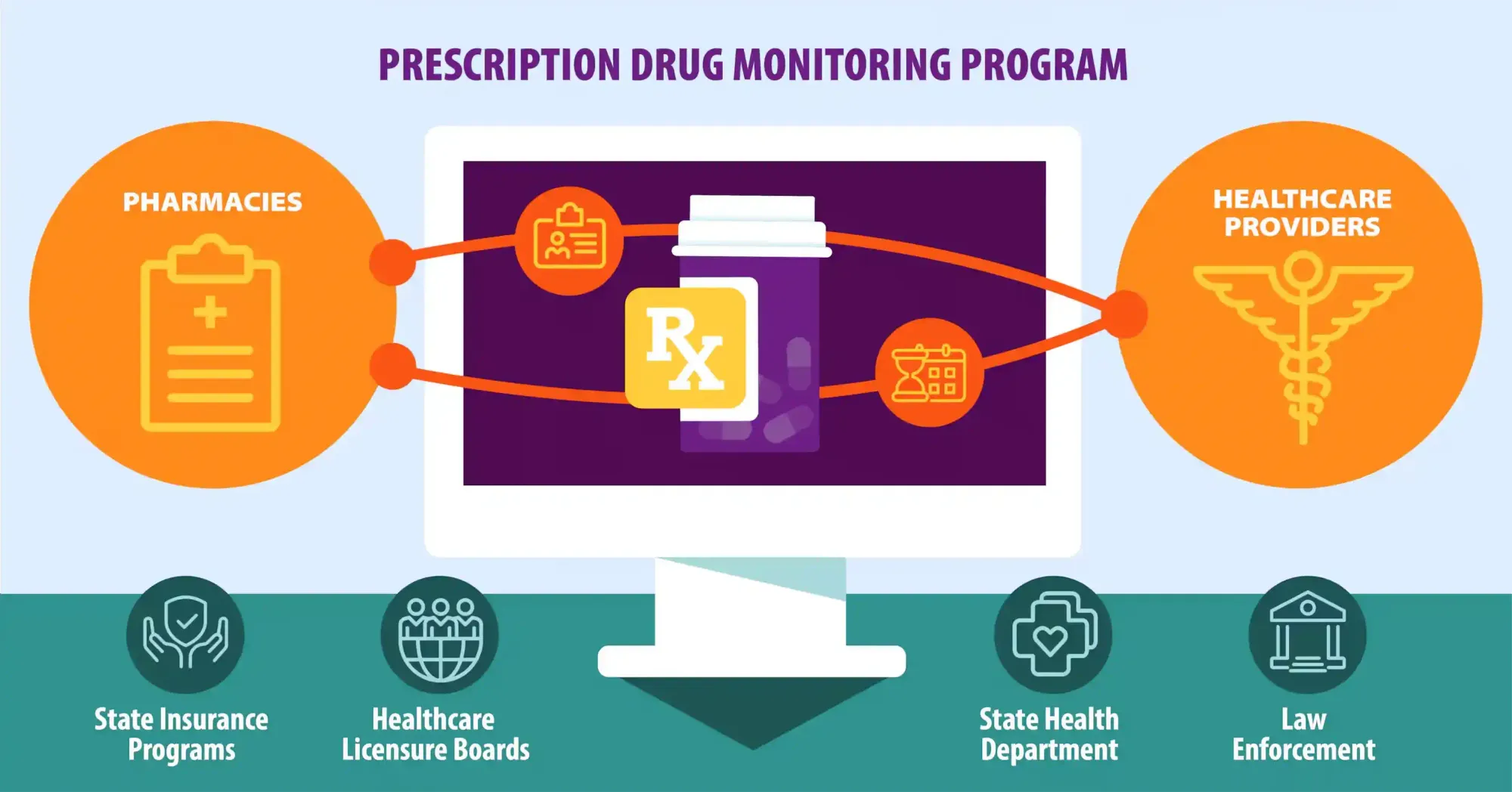
PDMPs have dramatically transformed the ways that investigators and prosecutors conduct cases against providers. New organizational developments paved the way for monitoring programs to have the greatest impact. Enforcement agencies’ impetus to investigate providers coincided with the arrival of technology that made those investigations easier and faster. Enforcement agents find both provider and patient data useful—the former because it shows patterns of providers’ behavior and the latter data because it helps law enforcement convince patients to become confidential informants in exchange for leniency in their own cases.
Healthcare providers have direct access to the database, but law enforcement access is more complicated. State laws restrict which enforcement agencies can get access and how. Some states give law enforcement direct access to data. In those states, enforcement agents have their own login to the system but can only legally access the data in the process of an active case, meaning that they are already investigating a specific crime. They can’t just search through the database to see what they find. Other states require law enforcement to request access from the agency that houses the PDMP, and the agency returns only information that is relevant to the case. Still other states require enforcement agents to obtain a warrant or a subpoena to access the data.16, 17 Regardless of how they get the information, PDMPs are a boon to law enforcement because they make tasks easier and more efficient.
Physician cases are reactive instead of proactive, which creates a barrier to starting an investigation. Enforcement agents say that they do not go out looking for bad doctors but find them through tips they receive from a patient, a parent, a healthcare provider, or another agency. They use information from tips to gather evidence and determine whether the case is worth pursuing. For a provider to come under law enforcement scrutiny, someone has to notice their behavior, feel compelled to do something, and know who to call.
The legwork necessary to investigate a physician traditionally posed a second barrier because investigators had to travel from pharmacy to pharmacy to gather the physician’s prescriptions. Now, thanks to the PDMP, that legwork has become deskwork. Instead of spending time on a potentially fruitless pharmacy expedition, enforcement agents simply look up the physician in the database or request access to information from the agency that controls it. Investigators can obtain a physician’s prescribing history, analyze prescribing patterns, and link their findings to other databases without setting foot outside the office.
Physician cases are decidedly unsexy. There are no drugs. There are no guns. There is paperwork. Stacks and stacks of paperwork.
PDMP data are a starting point. They do not make a case alone. Investigators examine the data from various angles and try to come up with alternative explanations for the patterns they see.
PDMPs also have their drawbacks. Investigators can use the database to track physicians, but a smart criminal physician also uses the database to monitor their patients and identify potential undercover investigators. People who are addicted to or diverting medications usually have a long PDMP report because they are actively trying to obtain opioids from various physicians. Undercover agents do not have a report at all, so running a report is a way to root out narcs. Knowing this, law enforcement finds ways to create fake reports so that they blend in with other patients. Overall, PDMPs benefit law enforcement because they improve the speed and accuracy of their investigations. Better investigations lead to more successful prosecutions (that is, a greater percentage of convictions).
The War on Drug Doctors
Drug cases capture media attention for a reason. Whether on popular TV shows or the evening news, drug cases are sexy. Towering bags of confiscated drugs and arrays of automatic rifles captivate audiences. This stagecraft also helps to justify the War on Drugs. Props such as drugs and guns show that the “bad guys,” the drug dealers, are armed and dangerous. They also show how desperately we need the “good guys,” the investigators and prosecutors, to keep the bad guys off the street.

By comparison, physician cases are decidedly unsexy. There are no drugs. There are no guns. There is paperwork. Stacks and stacks of paperwork. Not only do prosecutors have to prove to judges and juries that doctors—professionals revered as pillars of our society—are criminals, but they have to do so using something as uninspiring as paperwork. It’s a tough sell.
This essay was excerpted and adapted by the author from Policing Patients: Treatment and Surveillance on the Frontlines of the Opioid Crisis. Copyright © 2024 by Elizabeth Chiarello. Reprinted by permission of Princeton University Press.